By Richard N. Sater
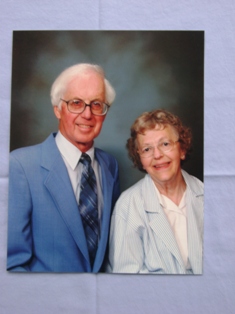
My wife, Dolores, may have been small in stature but she was great in heart.
I know. We were married for almost 54 years before she passed away in 2012 from complications of Parkinson’s Disease, after more than a decade of courageous battle against it.
An active and vital woman, Dolores wore many hats: wife, mother, grandmother, friend, and neighbor.
 The most important aspects of her life were her family and her faith. She didn’t make a big deal out of them – she just lived them to the fullest. She loved being outdoors in her flower gardens or walking the neighborhood with our dogs. She volunteered regularly at our church, the local hospital, the public library, and Meals-on-Wheels. She served as a Girl Scout leader for many years while our daughters were involved in the program. We enjoyed downhill skiing and hiking and bicycle riding together. An excellent cook and baker, she also kept a beautiful home for us.
The most important aspects of her life were her family and her faith. She didn’t make a big deal out of them – she just lived them to the fullest. She loved being outdoors in her flower gardens or walking the neighborhood with our dogs. She volunteered regularly at our church, the local hospital, the public library, and Meals-on-Wheels. She served as a Girl Scout leader for many years while our daughters were involved in the program. We enjoyed downhill skiing and hiking and bicycle riding together. An excellent cook and baker, she also kept a beautiful home for us.
Sometime in the year 2000, she started feeling that something was wrong. She went to see our family doctor and he sent her to a neurologist, who suspected Parkinson’s. He confirmed his diagnosis with tests, and immediately started her on medication to control the effects of the disease. The news was a serious blow – to all of our family.
For the first few years, the Parkinson’s didn’t have much impact on her ability to live a normal life, but gradually the disease started to take its dreadful toll. She started losing her ability to do things but never lost her spirit or desire to do everything that she could. This is a story of what we went through and the adjustments that we made to provide the best life for her that we could. It wasn’t easy – dealing with a debilitating illness never is. Much trial and error went into the process. For me, the easiest part was my decision to provide as much care as I could for the woman that had given me so much love over the years we spent together.
We quickly realized that we were not going to be able to keep living in our home of nearly thirty years. It had too many levels and stairs everywhere. There was also too much property for me to manage in addition to caring for her. We wound up building a new home that had everything on one floor (plus a basement that had an office, a workshop, exercise space and storage), with only a minimum of stairs to enter the house. The house was designed so that it could be customized for wheelchair access and the installation of a lift to access the basement if necessary.
We chose carpets with very short pile and eliminated throw rugs to minimize tripping hazards and facilitate easy movement of a walker (and later, a wheelchair). Initially, things continued as they had been in our other home, but as the disease progressed, we had to make adjustments in the way we lived day-to-day.
The first major impact was that she started to have difficulty keeping her balance and fell several times, sometimes injuring herself. I learned where she was most vulnerable and started making changes to help keep her safe. I installed several grab bars and a couple of extra railings in the bathroom and other potentially dangerous places. I put a fold-down seat in the shower to facilitate bathing. I considered installing special door locks for the basement stairway but decided that would not be necessary.
Short-term memory problems came next, and I realized that Dolores had difficulty remembering what she could do safely – even simple things like bending over to pick up something from the floor could be dangerous because her balance was so unsteady. On a few occasions, she went outdoors by herself – and fell in the yard and could not get up without help. She simply couldn’t remember not to do such things that she had always done. It frustrated both of us. I needed to find ways to keep her safe when I could not be close by her.
I was able to set up our home alarm system to sound if an outside door was opened. I found out about a seatbelt alarm that could be installed on almost any chair. If she opened the buckle on the seatbelt, an alarm sounded, and I could get to her before she got into trouble. I also installed a second seatbelt on the wheelchair that buckled in the back so she couldn’t reach it. She didn’t like the restriction, but I did what I had to do to keep her safe. (I learned that such restraints can’t be used in most care facilities unless a doctor’s letter is on file stipulating that the restraint is necessary for the resident’s safety.)
I found that using a baby monitor was helpful when she was in bed. With the monitor, I was able hear her if she needed something or wanted to get out of bed.
As the Parkinson’s grew worse, our world changed. Accomplishing the routine activities of our lives took more planning than I had been accustomed to – things like grocery shopping, meal planning and preparation, housecleaning, and laundry. Dolores always took pride in doing these things without help, but gradually, I had to take over all of these tasks. As often as possible, I used her as a resource to help me accomplish tasks that she had managed by herself for our entire married life. I made sure that she was involved in all decisions that affected her. Even little things, such as what clothing to wear, helped her outlook on life. Of course she wanted to feel good about how she looked!
I tried to be creative and not get hung up on the way things were always done in the past – a daily challenge for us … sometimes a valley to cross and sometimes a mountain to climb. It was essential for me to pay attention to how she was managing to do things for herself and to provide assistance if she had to struggle too much. She started requiring help with routine activities – things we don’t even think about – like using the toilet, bathing, getting in and out of bed, dressing, just getting around.
I remember a comment that she made when we were returning from out honeymoon. She had just realized that now she was the homemaker and kitchen manager. She had never filled those roles before. I knew my way around a kitchen but cooking was not one of my favorite activities. Dolores continued with her employment for a few months and during that time we worked together in the kitchen. After that, she took over and became and excellent cook and home manager. Now I was faced with the responsibility for those activities. I tried to remember the foods that Dolores especially liked (or disliked) and tried to include her favorites on a regular basis. When possible, I included her in the meal preparation, even if she could not do more than set the table or dry the dishes (nothing breakable or heavy) as I washed. It was important for her to contribute what she could – and a trial to convince her that she could no longer use the stove and oven safely.
Parkinson’s Disease affects motor coordination and muscle control, and Dolores developed problems with speech and swallowing. Some of her food had to be pureed for her to be able to consume it safely. I purchased a small food processor that helped a lot. On the advice of an occupational therapist, I found special eating utensils and dishes that made it easier for her to feed herself, although she eventually needed assistance to eat some meals.
Bibs and aprons helped protect her clothing. She felt better if she could leave the table without wearing her food. She enjoyed ice cream and other snacks, and I made sure they were always on hand – anything to brighten up an afternoon or an evening. When swallowing liquids became a problem for her, I learned about a readily-available product from a speech therapist, that could be added to beverages to thicken them enough to make them safer for her.
Keeping a clean house was important to both of us. In the early stages of the disease, Dolores hired someone to do the heavy cleaning about once a month. As time went on, we increased the frequency of the visits to weekly, and we added other chores so that I could focus on the care issues without giving up the home cleanliness that we wanted. Still, as much as possible, I let her help. Even little tasks, like folding and sorting laundry, helped her feel as if she could still take an active part in running the household.
As the disease progressed, her medications increased as well – a variety of pills to be taken at each meal and bedtime. We started out by managing her medications together, but over time, I took over that task as well. I needed to be sure that adequate quantities of each medication were on hand and prepared weekly. More importantly, I had to make sure that she took them at the appropriate times. When swallowing became a problem, I had to crush some of the pills and combine them with pudding or another easily-swallowed food. (Some medications could not be crushed, however.)
Equally important to our daily routine was fresh air and a change of scenery. Dolores spent so much time indoors (and later, confined to her wheelchair) that I had to make sure we got outside and away from home as much as possible. She and I both needed regular exercise – for rehabilitation and just to maintain her strength and mobility. We learned, from physical therapists, what exercises were appropriate and how and how often they should be done. I purchased some specific exercise equipment suitable for her use. Caregivers and our children and grandchildren were taught how to assist with the exercises, a win-win situation. Our children were pleased to be able to assist their mother and grandmother and it gave me a break too.
I learned gradually that I could not provide all of Dolores’s care 24 hours a day, seven days a week. I needed some relief. Friends suggested adult daycare, and I checked out a couple of facilities in our area that provided such services. During the last year of her life, I took her to daycare about two or three half-days a week. I also hired a caregiver to stop by most mornings to assist with bathing, dressing, and hair brushing. The caregiver was a godsend – she and Dolores chatted like old friends, and my wife got a break from me!
When I dropped her off at the daycare facility, I made sure we shared a kiss, and I always made a commitment about what time I would return to her. I knew she would get anxious if I did not arrive when she expected me. With her short-term memory problems, I never knew for sure if she remembered why I left her or when I would return. That is a problem I never could solve.
I did my best to pay attention to her world as it became more limited. I tried to be aware of the new challenges she faced. She loved to read the newspaper every morning, and when she could no longer hold the pages, I built a special table on wheels that she could use while seated in her favorite chair. It was big enough to support the newspaper. An optometrist helped us pick out reading glasses with extra magnification to help her continue to read – one of her favorite activities. Early on, I made sure she had books to read that were easy to follow and did not require a lot of concentration. (She particularly enjoyed the animal stories by veterinarian James Herriott.) I also installed a support on the side of her chair to help keep her upright when seated.
I tried to find other ways to keep Dolores entertained. Because short-term memory was a problem, I chose TV shows or DVDs that didn’t require following a plot line. Musical programs or variety shows worked well. Our son gave us the complete series of That’s Entertainment, three movies of excerpts from MGM musicals. We both enjoyed a National Geographic series on the National Parks (some of which we had visited together in years past) for the beautiful scenery.
Dolores really enjoyed gardening, and she missed it most when she could no longer get out among her flower beds. I set up a small table in the yard so she could work with potted plants. I encouraged visits by friends and family. Even when she had difficulty communicating herself, she could enjoy listening to others’ conversations and hear what people were doing. Eucharistic ministers from our church came to visit regularly, bringing her Communion, prayers, and a church bulletin, as well as keeping her up-to-date on the church gossip!
We traveled together for as long as we could, making occasional trips to our older daughter’s home in Virginia. Frequent stops were necessary for restroom breaks. I learned through experience that travel agencies could not always be trusted to ensure handicapped-accessible rooms would be available at motels. I carried a safety mat with us for the tub and some suction-cup grab bars to use in the bathroom as well. When long car rides became too difficult, we continued to make short trips. Our younger daughter lives close by, and we went to her home regularly – and she stopped by regularly (bringing four grandchildren) to visit and assist.
Speaking of car travel: gradually, Dolores reached a point where she could not sit up straight and would fall over sideways when restrained by the regular seatbelt and shoulder belt. I learned about a special car seat designed for small adults that included a four-point harness similar to those on child safety seats. I ordered the special seat through a medical supply store. With it, she was able to sit upright in the car – and travel much more comfortably as a result. (It also minimized the risk of injury if the airbag ever deployed.) I built a stool to help her step up into the car and covered the seat with a slippery fabric to make it easier for her to get in and out of the vehicle.
I had to pay special attention to what was going on with Dolores, looking for sudden changes in her abilities or behavior. Even an unfamiliar odor could alert me to a potential problem. Dolores had her share of medical emergencies, including at least one mini-stroke, pneumonia and repeated urinary tract infections. Each required special medical attention and occasional hospitalization. I learned to trust my own judgment – and not to listen when she assured me that everything was fine. If I felt that it was necessary, I took her to the emergency room or called for an ambulance immediately.
I had to be sure that I was not so busy taking care of her that I neglected to be her husband. We were still partners, and she looked forward to joint activities or just being together in a comfortable environment. We worked jigsaw puzzles together. I read to her – again choosing reading material that would not exceed her ability to follow the story. Sometimes we could combine activities to make them even more rewarding – like reading outside under a shade tree or on the front porch, where we could get some fresh air at the same time. We were a familiar sight in the neighborhood, touring around the block regularly, at first walking, then with her walker and later in the wheelchair. She always looked forward to greeting the neighbors as we passed.
Physical intimacy was always a regular part of our lives and it was important for it to continue. It showed her that she was still needed and a desirable partner. It continued to meet some of my needs as well. Sometimes this activity caused a little inconvenience, a small price to pay for the emotional benefits we gained.
Apart from practical care considerations, there were other important matters that we could not ignore. We had previously prepared Living Will and Medical Power of Attorney documents for each of us. They had to be witnessed and notarized. The first one defined the limits on health care that we were willing to accept in a crisis situation. The second defined the procedures for transferring health care decisions to another party when either of us became incapable of making those decisions for ourselves. These documents relieved any caregiver of the need to make critical health decisions on our behalf. I made sure that all of those assisting us with caregiving (and our daughters and son too) were aware of the Living Will stipulations and had access to a copy of those instructions.
On my own, I had to make the difficult choice about what to do when and if I could no longer care for Dolores at home. I had to choose a fulltime care facility, just in case. On several occasions during her last few years, she needed rehabilitation care after hospitalization for illness or injury. (A bout of pneumonia left her so weak that her doctor recommended recuperation at a care facility for several weeks before she could return home.) A local care facility had a space for her, and she moved in temporarily. As a result, we were familiar with the place, its staff, the programs and activities for its residents, the quality of the food, and so on. It would have been a difficult decision to move her there with little likelihood of ever being able to bring her back home, but I knew I might be faced with such a choice and decided it was better to be prepared.
Though no one likes to think about such things, we also needed to take care of some end-of-life decisions. Did we want a funeral? Cremation? A service? We attended a seminar offered through our church about end-of-life planning, which helped us make some of those hard choices so our children would not have to. I feel fortunate that Dolores and I were able to make satisfactory plans while she was still able to participate in the decision-making process.
Before anyone can care for an ailing spouse, he or she, needs to take care of themself and look to their own well-being. I could not help Dolores if I was ailing myself. That meant getting a flu shot every year, taking all of my own medications, exercising regularly, and getting regular physical check-ups. Once, Dolores fell when going down the two steps into the garage. I tried to catch here and in the process, fell and tore one of my rotator cuffs. I needed to have surgery (as well as a month of recuperation time and physical therapy) to fix the problem. To manage this crisis, I had to rely on the help of others. My son came from his home in Seattle to stay with us for a month to care for both of us, and Dolores spent a few weeks in an assisted-living facility until I was sufficiently healed so that she could return home. Overall, I feel very lucky that nothing more serious happened to me.
***
This story has been about my experiences in helping my wife live the best kind of life that she could, in spite of the ravages of Parkinson’s Disease. My experience was unique, but the challenges I faced may be common to anyone in a similar situation. I tried to identify problems and issues as they came up and dealt with them in the best way that I could.
Only you can decide if providing home care for an ailing spouse is the right choice for you and the best choice for your wife or husband. When there is no more care to be given, the best that you can hope for is the comfort that you did everything you could.
Making home care work requires a commitment from both partners. If either partner cannot commit, don’t even attempt to do it – find someone or some place that can provide the necessary care. Don’t let it become a point of disagreement. Even under the best of circumstances, it is frustrating and challenging. I tried to do my best in dealing with those issues.
At that end, I believe we were approaching the time when I could no longer provide the full care that Dolores needed. She was having more and more difficulty speaking and making her needs understood, and our situation had become more of a struggle. I had not made any arrangements for her to move into a permanent care facility but that time was approaching. She died unexpectedly of a heart attack in June 2012.
Nothing could have prepared me or our family for such a thing.
Caring for Dolores truly was a labor of love. I believe we grew closer than we had ever been before. It is the hardest work I have ever done, but in some ways, the most rewarding.
Written by: Richard N. Sater
August 6, 2013

Follow us on